
During a TMS treatment session, you are seated and reclined in a comfortable chair. You are fully awake and alert, and you can talk, listen to music, watch videos, or relax with earplugs. Earplugs or earbuds are used to minimize the clicking sound of the equipment. There are no new medications involved in a TMS treatment; most patients continue on the ones they were regularly taking before starting TMS therapy. One of our TMS doctors or TMS technicians rests the magnet coil on the appropriate area of your head before starting the session. You will need to remove any metal hair clips, hearing aids, or facial piercings before each session. A typical treatment session lasts about between 20 and 30 minutes, during which time you will feel a series of taps on your head under the TMS coil. Some patients may experience mild discomfort on their scalp under the coil or have a residual headache after the first few sessions. Both of these are common, can be managed with adjustments to the stimulation, and typically resolve within the first week of daily sessions.
The Butler Hospital TMS Clinic consists of an experienced team of TMS-credentialed doctors, TMS-certified technicians, and a TMS nurse clinician, all trained in the delivery of TMS therapy.
A TMS doctor will be involved in all phases of your TMS therapy including:
Your outpatient psychiatric medication prescriber will remain involved in your care during your course of TMS therapy and will continue to meet with you and prescribe your medications during your course of TMS therapy. TMS doctors at Butler Hospital will not typically prescribe any medications for you, but they will coordinate care with your outpatient prescribers to ensure that your care is integrated and safe.
If you are engaged in outpatient psychotherapy, you do not need to stop it during TMS.
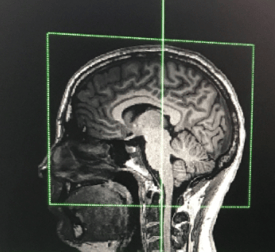
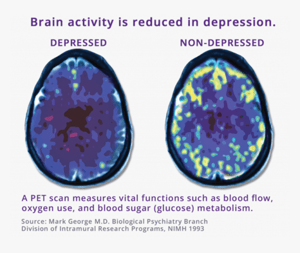
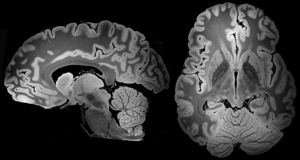
TMS is a treatment for depression that works by directly stimulating the brain. TMS activates certain parts of the brain by using electrical energy passed through a coil of wires to create a powerful magnetic field. During a TMS treatment session, energy from this magnetic field is transferred into a patient's brain when the coil device is applied to a person’s head. Concentrated magnetic energy passes easily through skin and skull, activating the brain painlessly and without surgery or sedation. TMS is applied to areas of the brain associated with mood regulation. TMS effects chemical activity and function of mood regulation structures in the brain, resulting in symptom improvements in depressed patients.
During the treatment you are seated and reclined in a comfortable chair. You are fully awake and alert, and you can talk during the treatment. There are no new medications involved in a TMS treatment; most patients continue on the ones they were regularly taking before starting TMS therapy. The TMS doctor or clinical technicians rests the magnet coil over the appropriate area of the scalp before starting the session. You will need to remove any metal hair clips, hearing aids, or piercings before the treatment. Usually patients wear earplugs or listen to music during treatment to minimize the clicking sound of the equipment. A typical treatment lasts between 20 -30minutes, during which time the patient feels a series of taps on their scalp.
As with medications, the time to respond to TMS will vary between individuals. It is recommended that patients receive TMS treatments every weekday, for four to six weeks to obtain the most successful TMS treatment for depression. Often there is no noticeable mood change during the first few weeks. In the clinical trials, a small percentage of patients required more than 30 treatments to experience relief from depressive symptoms. Others noticed significant benefits from TMS at the end of the second week of TMS treatments. At Butler Hospital, TMS sessions are scheduled in 1 hour blocks.
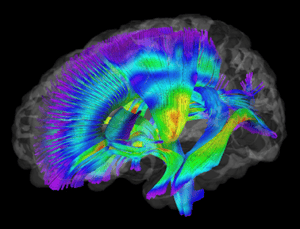 One of the benefits of TMS, relative to other depression treatments, is the accuracy it achieves in working on the desired brain region, or “target.” TMS allows clinicians to target very specific parts of the brain, leaving other areas alone. TMS does not lead to memory difficulties or other impairments in thinking. It does not change a person’s personality, though when patients experience relief from symptoms of the depression, their ability to think and function typically improves.
One of the benefits of TMS, relative to other depression treatments, is the accuracy it achieves in working on the desired brain region, or “target.” TMS allows clinicians to target very specific parts of the brain, leaving other areas alone. TMS does not lead to memory difficulties or other impairments in thinking. It does not change a person’s personality, though when patients experience relief from symptoms of the depression, their ability to think and function typically improves.
No, TMS is not the same as electroconvulsive therapy (ECT). ECT, commonly referred to as “shock therapy,” is a treatment for depression that uses electricity to produce seizure-like activity in the brain while a patient is “asleep” under anesthesia. TMS is similar to ECT by virtue of its direct brain stimulation method to relieve depression. However, TMS is a treatment performed in the awake/alert patient; no anesthesia or sedation is needed. Magnetic energy, rather than electricity, is applied to the scalp during TMS.
During the first few treatments, the tapping sensation on your scalp may be uncomfortable. Up to 50 percent of patients who receive TMS will experience some mild to moderate soreness on their head during the first week of treatment. Over-the-counter pain medicines such as aspirin, Tylenol or Motrin can be used, before or after TMS sessions, to manage the discomfort. Over time, the scalp becomes less sensitive to the tapping sensation of the magnetic pulses and the treatment does not produce discomfort.

TMS is relatively free of side effects, compared to other treatments for depression. Studies show that about one in five people will develop a mild to moderate headache or scalp soreness after they receive TMS, but this should subside after the first week and it can be well managed.
Not necessarily. This is decided on an individual basis. During your pre-treatment consultation evaluation, the doctor will discuss this with you; provide recommendations about use of medications during TMS therapy at Butler Hospital.
Once you have reviewed the information on this website, you may have a better idea if TMS is a treatment consideration for you. You can begin the screening process by calling (401) 455-6632 to begin the screening process and speak with a member of our TMS team. We will then ask you to complete some forms asking more information about your demographics and treatment history prior to being scheduled for a consultation with one of our TMS physicians.
 The Butler TMS Clinic has been a national leader in advocating for insurance coverage and expanding patient access to TMS therapy. Medicare, Medicaid, and all commercial insurances cover TMS therapy for appropriately selected patients. Some patients may have co-payments for TMS services, and we will provide information to help you determine what your copays might be.
The Butler TMS Clinic has been a national leader in advocating for insurance coverage and expanding patient access to TMS therapy. Medicare, Medicaid, and all commercial insurances cover TMS therapy for appropriately selected patients. Some patients may have co-payments for TMS services, and we will provide information to help you determine what your copays might be.
Copyright © 2026 Care New England Health System